May 14, 2021 | By Jill Young, CPC, CEDC, CIMC
The time has come for you to consider the “new time” method to determine the evaluation and management (E&M) coding for your office and other outpatient services. I use the phrase “new time” to differentiate it from the “old time” concept you are accustomed to working with. The concept is that time is used to select the level of service when counseling and/or coordination of care dominates (greater than 50%) of the total time of the visit. This methodology will continue to be used on all other E&M services provided on or after January 2021 change. When you look at the “new time” concept to select the level of service for an office or other outpatient service, the following lists are offered for what is and is not included as an accepted activity:
“New Time” includes the following activities (when performed)
- Preparing to see the patient (e.g., review of tests)
- Obtaining and/or reviewing separately obtained history
- Performing a medically appropriate examination and/or evaluation
- Counseling and educating the patient, family, or caregiver
- Ordering medications, tests, or procedures
- Referring and communicating with other health care professionals (when not separately reported)
- Documenting clinical information in the electronic or other health record
- Independently interpreting results (not separately reported) and communicating results to the patient, family, or caregiver
- Care coordination (not separately reported)
Do not count time spent on the following
- The performance of other services that are reported separately
- Travel
- Teaching that is general and not limited to discussion that is required for the management of a specific patient
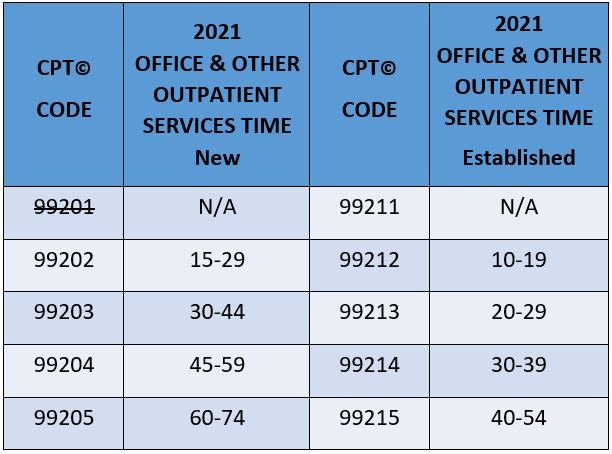
The time spent is the total time spent on the date of the encounter, including both face-to-face time and non-face-to-face time. This language is found within the new CPT code descriptors along with a range of time for each code (99202-99205 and 99212-99215).
Time spent by staff in preparing the patient to be seen or time spent by technicians (e.g., blood draw, taking of x-rays) is not counted. Additionally, time spent by the provider performing other billable services (i.e., x-ray or EKG interpretations, procedures) is also not included in the calculation of the total time of the visit for the day.
CPT does not have any specific guidance on how the time of the visit should be documented. A best practice is to make sure the total time of the visit is clearly documented to show the required of time associated with the selected code was met. It is not recommended that you give a time range (e.g., “20 to 29 minutes was spent with the patient”). My Medicare carrier (WPS) stated they were “highly recommending” notations of pre-visit, visit, and post-visit time be documented.
The guidance from the AMA discusses a split-shared visit. This is not the type of visit you are thinking of that still exists within the Medicare Carrier Manual for Inpatient Hospital Visits. The split-shared visit for Office and other Outpatient Services in 2021 is defined, by the AMA, as a visit in which “a physician and other qualified health care professional(s) jointly provide the face-to-face and non-face-to-face work related to the visit.” Unlike hospital visits where the documentation of the combined work of the two individuals determines the level of service, the split-shared visit for these services in 2021 is only used when time is used to determine the level of service. Two or more individuals from the office may discuss the patient, only the time of one individual should be counted. The overlapping time during discussion of the patient is only counted by one provider, the performing provider of the visit. Two examples:
- Physician’s Assistant (PA) reviews the record and sees a patient (10 minutes). PA leaves the room and has a discussion with the physician (5 minutes). PA goes back into the room and completes the service (15 minutes). Total time used to select the level of service to be billed by the PA: 30 minutes
- PA reviews the record and sees a patient (10 minutes). PA leaves the room and has a discussion with the physician (5 minutes). It is decided that the physician will now take over and see the patient. The physician enters the room and completes the service (15 minutes). Total time used to select the level of service to be billed by the physician: 30 minutes.
Documentation of the different segments of a patient’s visit, in summary along with the time for that segment, along with total time of the visit, will provide the information needed for the selection of the level of service and show medical necessity. The other provider in these examples does not separately bill for their time.
As always, be sure the documentation in addition to meeting the requirements of the level of service, either by utilizing the Elements of Medical Decision-Making table or by using time, shows the medical necessity of the visit. The narrative of the visit with free texting may well be the most efficient and effective way to meet both these requirements.
For your use, the following is a timetable for office and other outpatient services for 2021 for you to print and post where it would be most useful to you.