February 1, 2022 | By Sean Weiss, CHC, CEMA, CMCO, CPMA, CPC-P, CMPE, CPC
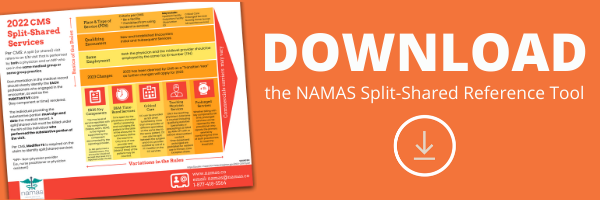
As 2022 kicks into full gear one of the biggest areas providers (*rendering services in hospitals) face a change is tied to the 2022 CMS Split/Shared Visit Rules and what the anticipated impact(s) will be (here is a link to the: 2022 Medicare Physician Fee Schedule (MPFS) Final Rule)
So, what is it in a nutshell that the Final rule actually says? First, there is a definitional change that took place which now defines a split (or shared) visit as “an E/M visit in a facility setting that is performed in part by a Physician and an NPP who are in the same group.” It is also important to keep in mind that the term Facility setting is synonymous with the term institutional setting as outlined in the Final Rule. There is a referenced regulation (§ 410.26(b)(1)), whereby institutions are limited to hospitals and skilled nursing facilities (SNFs) so keep that in mind. The 2022 MPFS Final Rule is the first time that a SNFs was added as a permitted location for Split/Shared Visits. The rationale for this is there would be close coordination and collaboration of care within groups.
The Final Rule also clarified that the Split/Shared Visit scenario does not apply to the office setting (Incident-to is still the driver here).
Let’s address the requirements:
- The 2022 MPFS Final Rule requires that the Split/Shared Visit encounter be billed under the provider who performed “the substantive portion” of the encounter.
- In the Final Rule, CMS intended to define the “substantive portion” of the encounter as being more than half of the total time dedicated to the patient encounter.
- The total time determination is defined similarly to the 2021 office-based coding requirements.
- Split/Shared Visit encounters can currently be billed under the involved physician as long as the physician’s “substantive” participation in the encounter was accurately documented in the medical record.
- The “Billing Provider” is required to be the one that signs and dates the encounter document. The encounter document must clearly indicate the physician and APP involved in the patient’s care and their roles in that care – this includes the individual time and/or effort dedicated to the encounter in sufficient detail to justify the “Billing Provider” determination.

Source: Table 26 of the 2022 MPFS, Fed Reg., pg. 65153
- Split/Shared encounter claims require a specific modifier irrespective of the provider type the encounter is billed under. This allows for the identification and tracking of the encounter. The designated modifier is “FS.”
- The Split/Shared criteria applies to new or established patients, initial and subsequent visits, critical care services, and prolonged services. This is a significant departure given the fact that in the past it only applied to established patient encounters.
- The biggest takeaway is this… If the NPP turns into the “Billing Provider” based on their performing the “substantive portion” of the encounter, based on total time spent, the NPP is thus awarded the payment (wRVUs). This will most likely not sit well with the physician since justifying their receipt of the payment would be difficult based on how the regulations are written and that based on the total time, they would not have provided the substantive portion of the encounter.
- This is going to be in the coming months and years a major audit target and you better be prepared to justify the billing under the physician through clear and concise documentation and capturing the total time spent by that physician as the controlling units.
Perform your internal or external audits to ensure compliance with the new regulations out of the gate to ensure you are not blindsided by Medicare or another payor recognizing these guidelines. This could prove to be a costly mistake if not managed properly out of the gate.