March 31, 2023 | By Pam Vanderbilt, CPC, CPMA, CPPM, CPC-I, CEMC, CDEO, CPB, CFPC, CRC, CPEDC, CEMA
President, Knowledge Tree Billing, Inc.
A lot happens in March! Spring officially begins — bringing with it new growth, Spring Break, and basketball fans across the country get bracket crazy with March Madness. In all the beauty and excitement, another March happening seemed to slide in quietly…the AMA Errata and Technical Corrections – CPT 2023.
On March 9, 2021, AMA released the technical corrections for the 2021 E&M guidelines. These included quite a few clarifications, which is understandable considering 2021 ushered in the most significant changes to E&M in over 25 years. January 1, 2023, brought an expansion of the guidelines to include the rest of the E&M services that are reported as levels of service, so was really not a surprise the March 1, 2023, would also bring come clarifications. What was surprising is how few clarifications there were. Maybe that is a result of how well auditors and documentation improvement experts have adapted and educated coders and providers on the correct use of the 2021 guidelines.
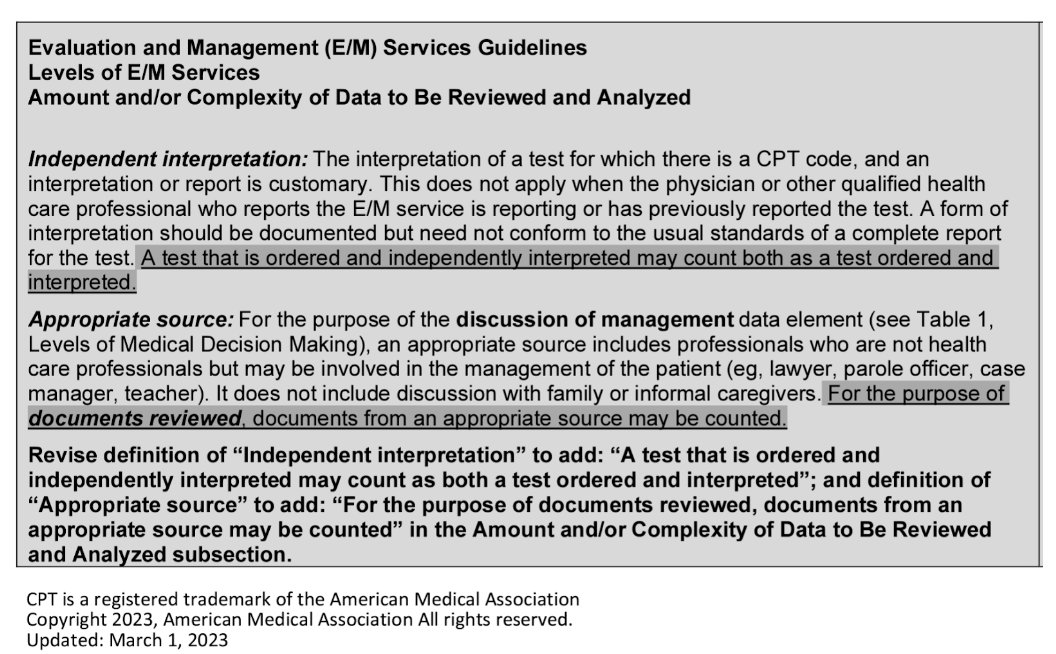
Included in the clarifications were modifications to the guidelines about independent interpretation and appropriate source. The following is a snippet of the document:
Since the Amount and/or Complexity of Data to Be Reviewed and Analyzed seems to be the column on the MDM table, it seems fitting the clarifications are both components of this column. Under moderate and extensive (high) risk, these are Category 2 and Category 3 data elements. I suppose I should say were, since the clarifications also identify we can give category 1 credit that we may not have prior to this year.
Clarifying that using information from an appropriate source that was obtained as a document instead of through a discussion makes sense. In fact, some of us already considered these as documents from a unique source. The clarification is confirmation we have been giving credit correctly. Think about our providers who specialize in ADHD treatments for pediatric patients; they will routinely request teachers to fill out a report about the patient’s behaviors and noted responses to treatment. These documents are reviewed to determine the effectiveness of the treatment plan in a more objective manner than just the history from the patient or their family members. We can now confidently give credit for review of these documents from each unique appropriate source.
If you are scratching your head about the clarification that we can give credit for both the order and the independent interpretation, you are not alone! This seems to be inconsistent with the definition of “analyzed” in the guidelines which allows us to give credit for either order or review, but never both.
Since we don’t have a rationale with the clarification, we don’t really know what the thought process is that allows us to give credit for both. Maybe it is the additional work of the provider in viewing the study and making their own interpretation as opposed to reviewing the interpretation of another. Regardless of the reason for this clarification, there are some concerns that come to mind with this change.
The first is that independent interpretation is already moderate complexity data without any other data being considered. Adding the credit for the order in Category One in addition to two other tests would cause our data to score as extensive, potentially causing our overall MDM to score to the highest level. Could this potentially send a message to providers to independently interpret a test to support a higher level of service?
The other concern that comes to mind is the pushback we get during provider education about how Category One data is scored. As mentioned before, we only give credit for order OR review, not both. We also only give credit for documents from each unique source, regardless of how extensive the documentation is. Think about the patient that is being seen by their PCP for follow-up after a three-week hospitalization; while in the hospital the patient was seen by multiple specialties and had multiple diagnostic tests that require the PCP’s review. There is a lot of information our PCP is reviewing, but it only scores as one review from a unique source. How will we educate our providers that the work of independent interpretation is different than the work of reviewing extensive records from a unique source?
Knowing AMA and their commitment to the provider community, we can be confident that a rationale will be forthcoming. Until then, we all need to update our policies to reflect how our organizations will handle the clarifications so the coders, auditors, providers, and administration are on the same page. Enjoy the madness!
https://www.ama-assn.org/system/files/2023-cpt-corrections-errata.pdf
Your next steps:
- Contact NAMAS for information about customized staff and provider training.
- Read more blog posts to stay updated on the 2023 Revisions to the 2021 E&M Guidelines.
- Subscribe to the NAMAS YouTube channel for more auditing and compliance tips!
NAMAS is a division of DoctorsManagement, LLC, a premier full-service medical consulting firm since 1956. With a team of experienced auditors and educators boasting a minimum of a CPC and CPMA certification and 10+ years of auditing-specific experience, NAMAS offers a vast range of auditing education, resources, training, and services. As the original creator of the now AAPC-affiliated CPMA credential, NAMAS instructors continue to be the go-to authorities in auditing. From DOJ and RAC auditors to CMS and Medicare Advantage Auditors to physician and hospital-based auditing professionals, our team has educated them all. We are proud to have helped so many grow and excel in the auditing and compliance field.
Looking to start up a medical practice or grow your existing practice? Contact our parent company, DoctorsManagement.