Most of you are familiar with the medical necessity of the E&M encounter prior to 2021 documentation guidelines. But how does that equate in 2021? Today, we’re going to talk about how to understand medical necessity and 2021 documentation guidelines in the auditing of your encounters.
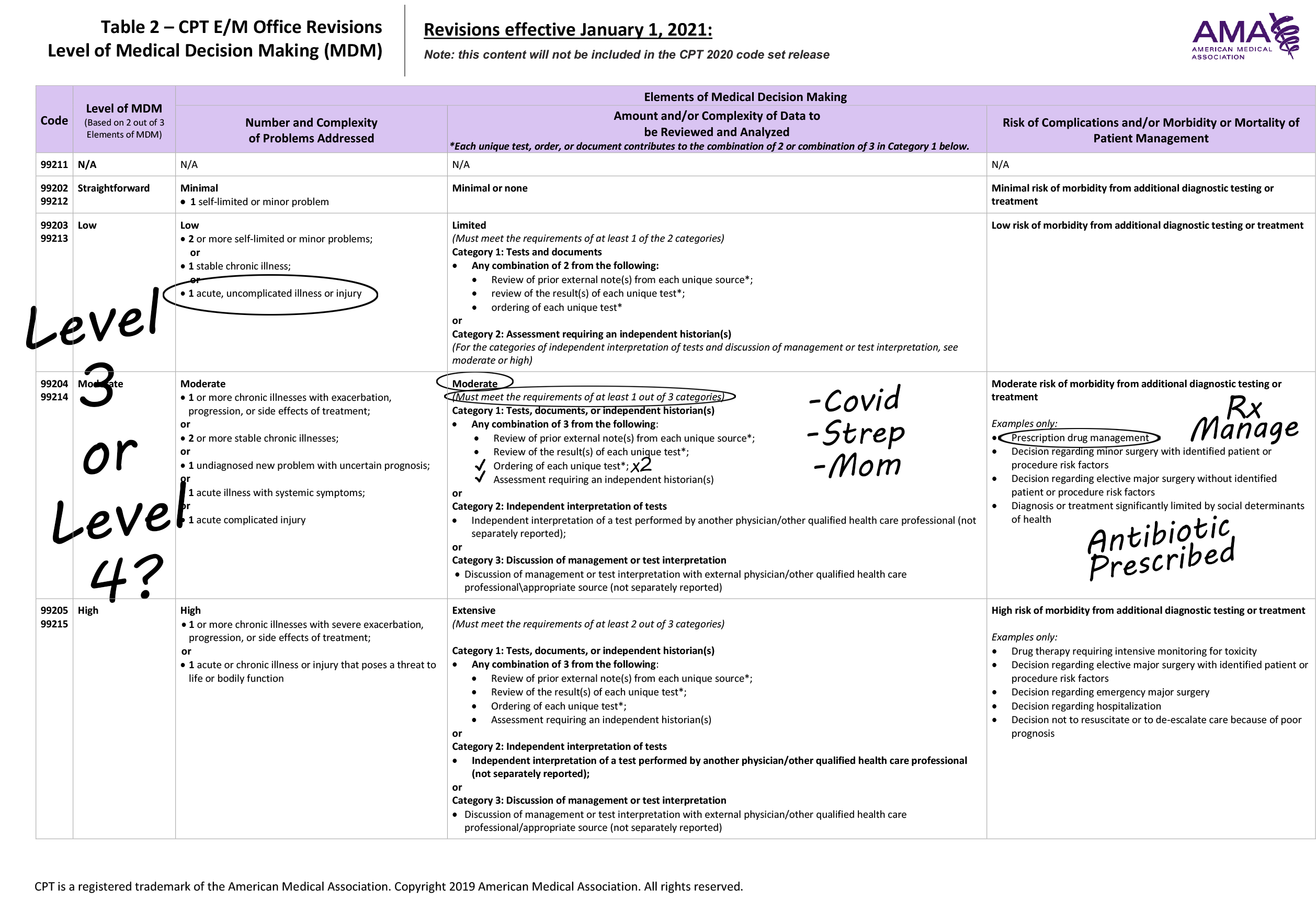
Let’s take a look at the medical decision making chart when we really have to consider risk associated with medical decision making. Let’s focus, if you will, on our MDM chart when it looks something like this:
(Click the image for a closer look)
Here we have a medical decision making chart where our presenting problem has scored low, a level 3, but yet our data has scored as moderate, scoring a level four, and our treatment plan has scored also as a level 4. According to our MDM documentation guidelines, technically we would score this as a Level 4. However, we have to consider medical necessity and say “but wait a minute, what about the presenting problem?” Do we weigh in the presenting problem and understand the risk associated with how the presenting problem plays into this and the medical necessity of that presenting problem? We know that the Centers for Medicare and Medicaid and the claims processing manual did not remove the language that says medical necessity is the overarching determining factor, so we should still be taking medical necessity into consideration. If we also look at the AMA documentation guidelines, we were given technical corrections as follows:
The term risk used in these definitions relate to the risk from the condition while condition risk and management risk may often correlate the risk from the condition is distinct from the risk of the management.
So, for those reasons, we should consider the risk of the condition in a different way than we consider the risk of the management. So, for the patient in our example, who maybe had strep throat; 1) we did do a COVID test, 2) a strep screen, and 3) we talked to mom. That gives us our three points for data. We also gave them an antibiotic for strep. At the end of the day, the acuity, the medical necessity of the presenting problem, is still strep throat. Does the complexity truly increase in treating that problem because this patient was tested for COVID, or because of strep screen was also done, or because mother was talked to? Because one of those three issues is what raise this value to a new level of service. So, you within your organization need to have a policy here. This is truly one of those grey areas. I can’t tell you the secret sauce. No one can tell you the secret sauce because inside these published guidelines, there’s no more of an answer than what we just read. The risk is the risk of the condition and sometimes it will correlate to the management, but sometimes it won’t. So, what’s your policy? Are your coders and auditors coding and auditing this situation the same? If you had 5 team members, looking at this chart right now, would you have two that said it’s a level 3 and three that say it’s a level 4, or would you have five team members that scored it all the same? That’s what you want on your team, so be sure that you have your team members cohesively auditing things the same way and coding things the same way…and you do that by creating the policy.
Visit the NAMAS YouTube channel to view the video of Shannon DeConda discussing this topic.